Scleritis
Symptoms
Severe and boring eye pain (most prominent feature), which may radiate tothe forehead, brow, or jaw, and may awaken the patient at night. Gradual oracute onset with red eye and decrease in vision. Recurrent episodes are common.Scleromalacia perforans may have minimal symptoms.
巩膜炎
症状:
严重的烧灼感的眼痛是最显著的症状,可放射到前额、眉弓或颌部,患者夜间常被痛醒。以渐进性或急性眼红和视力下降起病。易复发。穿通性巩膜软化的症状轻微。
Signs
Critical. Inflammation of scleral, episcleral, andconjunctival vessels (scleral vessels are large, deep vessels that cannot bemoved with a cotton swab and do not blanch with topical phenylephrine) can besectoral or diffuse. Characteristic bluish scleral hue (best seen in naturallight by gross inspection). Scleral thinning or edema may be present.
主要体征:
巩膜、表层巩膜和结膜的血管炎症呈扇形或弥散性。巩膜血管粗大、较深,不能被棉棒推动,滴用去氧肾上腺素不能使之收缩变白。巩膜呈特征性蓝色(在自然光下肉眼可查见)。可有巩膜变薄或水肿。
Other. Scleral nodules, corneal changes (peripheralkeratitis, limbal guttering, or keratolysis), glaucoma, uveitis, or cataract.
其他体征:
巩膜结节,周边部的角膜炎、角膜缘呈沟状或角质层分离等角膜病变,青光眼,葡萄膜炎,白内障。
Other Signs of Posterior Scleritis. Subretinalgranuloma, exudative retinal detachment, proptosis, or rapid-onset hyperopia.
后巩膜炎的其他体征:
视网膜下肉芽肿、渗出性视网膜脱离、眼球突出、急性起病的远视。
Differential Diagnosis
•\tEpiscleritis: Sclera not involved. Blood vesselsblanch with topical phenylephrine. More acute onset than scleritis. Patientstend to be younger and have very mild symptoms, if any. See 5.6, Episcleritis.
鉴别诊断:
表层巩膜炎:巩膜不受累。滴用去氧肾上腺素使其血管收缩变白,与巩膜炎相比,起病急。好发于年轻人,症状较轻。参见本章第六节表层巩膜炎。
Etiology
Fiftypercent of patients with scleritis have an associated systemic disease. Work-upindicated if no known underlying disease is present.
病因学:
50%巩膜炎患者伴有相关的全身疾病。如果原发病未出现临床症状,需要做一些检查以协助诊断。
More common. Connective tissue disease (e.g.,rheumatoid arthritis, Wegener granulomatosis, relapsing polychondritis,systemic lupus erythematosus, Reiter syndrome, polyarteritis nodosa, ankylosingspondylitis, inflammatory bowel disease), herpes zoster ophthalmicus, syphilis,status postocular surgery, gout.
较常见于 结蹄组织病,如类风湿性关节炎、Wegener肉芽肿、复发的多发性软骨炎、系统性红斑狼疮、Reiter综合征、结节性多动脉炎、强制性及、肠炎。眼部带状疱疹、梅毒、眼手术后、痛风。
(inflammatory bowel disease,炎症性肠病)
Less common. Tuberculosis, other bacteria (e.g.,Pseudomonas species with scleral ulceration, Proteus species associated withscleral buckle), Lyme disease, sarcoidosis, hypertension, foreign body,parasite.
2.较少见于 结核,其他细菌如假单胞菌属感染合并巩膜溃疡、巩膜扣带并发的变形菌属感染,莱姆病,结节病,高血压,异物,寄生虫病。
Classification
1 Diffuse anterior scleritis: Widespread inflammation of theanterior segment.
2 Nodular anterior scleritis: Immovableinflamed nodule(s). See Figure 5.7.1.
3 Necrotizinganterior scleritis with inflammation (see Figure 5.7.2): Extreme pain. Thesclera becomes transparent (choroidal pigment visible) because of necrosis.High association with systemic inflammatory diseases.
4 Necrotizinganterior scleritis without inflammation (scleromalacia perforans): Typicallyasymptomatic. Mainly seen in longstanding rheumatoid arthritis.
5 Posteriorscleritis: May start posteriorly, or rarely be an extension of anteriorscleritis, or simulate an amelanotic choroidal mass. Associated with exudativeretinal detachment, disc swelling, retinal hemorrhage, choroidal folds,choroidal detachment, restricted motility, proptosis, pain, tenderness. Usuallyunrelated to systemic disease.
分类:
1.弥漫性前巩膜炎 眼前节弥漫性炎症。
2.结节性前巩膜炎 固定的炎性结节。见图5.7.1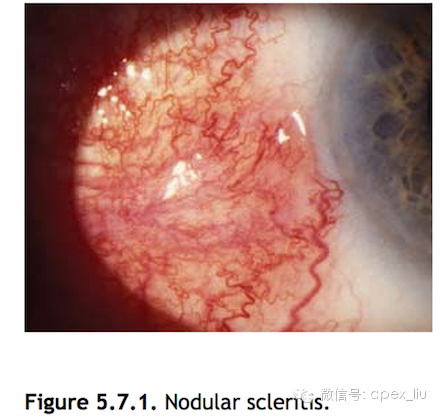
3.坏死性前巩膜炎伴炎症反应(见图5.7.2)
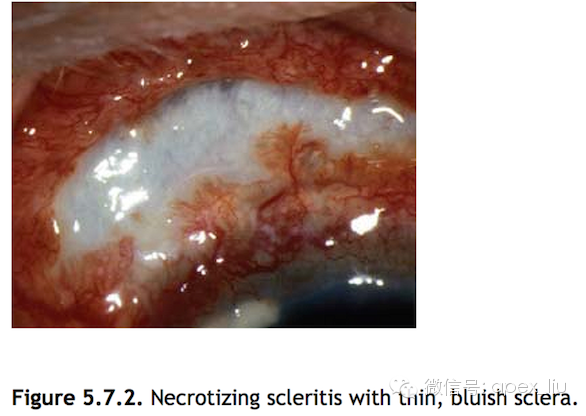
1)极度疼痛。
2)由于坏死的巩膜变成透明,可见脉络膜色素。
3)与全身炎症性疾病密切相关。
4.坏死性前巩膜炎不伴有炎症反应(穿通性巩膜软化)
1)可没有症状。
2)主要见于长期的风湿性关节炎的患者。
5.后巩膜炎
1)可由后巩膜起病,个别病例是前巩膜炎的蔓延所致,或表现为类似无色素的脉络膜占位。
2)伴有渗出性视网膜脱离、视盘水肿、视网膜出血、脉络膜皱褶、脉络膜脱离。
3)伴有眼球运动受限、眼球突出、眼痛、眼触痛。
4)通常和全身疾病无关。
Work-Up
1 History: Previous episodes? Medical problems?
2 Examine the sclera in all directions of gaze by gross inspectionin natural light or adequate room light.
3 Slit-lamp examination with a red-free filter (green light) todetermine whether avascular areas of the sclera exist. Check for corneal oranterior chamber involvement.
4 Dilated fundus examination to rule outposterior involvement.
5 Completephysical examination (especially joints, skin, cardiovascular and respiratorysystems) by an internist or rheumatologist.
6 Complete blood count, ESR, uricacid, RPR, FTA-ABS, rheumatoid factor, ANA, fasting blood sugar,angiotensin-converting enzyme, CH 50 (total complement activity assay), C3, C4,and serum ANCA.
7 Othertests if clinical suspicion warrants additional work-up: PPD with anergy panel,chest radiograph, radiograph of sacroiliac joints, B-scan ultrasonography todetect posterior scleritis (e.g., T-sign), and magnetic resonance imaging (MRI)or CT scan if indicated.
检查:
1.病史 既往史?有无内科疾病史?
2.自然光或室内充足照明下在各个注视方位肉眼观察、检查巩膜。
3.裂隙灯下用无赤光检查巩膜 确定有无存在无血管区,检查角膜和前房有无受累。
4.散瞳检查眼底 观察有无眼后节受累。
5.请内科专家或类风湿病学专家做全面体检 尤其注意关节、皮肤、心血管和呼吸系统。
6.全血计数、血沉、快速血浆实验(RPR),螺旋体抗体吸附荧光测定试验(FTA-ABS),类风湿因子,抗核抗体,空腹血糖,血管紧张素转换酶,血清总部提,补体C3和C4,血清抗中性粒细胞胞浆抗体。
7.如临床体检疑有某些疾病,应行以下检查 纯蛋白衍生物和无反应性嵌合板,胸片,骶髂关节X线片,B超探查后巩膜炎(如T征),磁共振或CT扫描。
Treatment
1 Diffuse and nodular scleritis: One or moreof the following may be required. Concurrent antacid or histamine type 2receptor blocker (e.g., ranitidine 150 mg p.o., b.i.d.) is advisable.
—NSAIDs (e.g., ibuprofen 400 to 600 mg p.o., q.i.d.;naproxen 250 to 500 mg p.o., b.i.d.; indomethacin, 25 mg p.o., t.i.d.): Threeseparate NSAIDs may be tried before therapy is considered a failure. If stillno improvement, consider systemic steroids.
—Systemic steroids: Prednisone 60 to 100 mg p.o., q.d.for 1 week, followed by a taper to 20 mg q.d. over the next 2 to 3 weeks,followed by a slower taper. An oral NSAID often facilitates the tapering of thesteroid. If unsuccessful, consider immunosuppressive therapy. See “Prednisone” in Pharmacopoeia beforeprescribing systemic steroids.
—Immunosuppressive therapy (e.g., cyclophosphamide,methotrexate, cyclosporine, azathioprine): If one drug is ineffective or nottolerated, additional agents should be tried. Systemic steroids may be used inconjunction. Immunosuppressive therapy should be coordinated with an internistor a rheumatologist. The role of topical cyclosporine drops is unclear.
治疗:
1.弥漫性和结节性巩膜炎 以下一个或多个治疗可供选择,建议联合应用抗酸剂和H2受体阻滞剂,如雷尼替丁150mg,口服,日2次。
1)非甾体类抗炎剂 布洛芬400-600mg,口服,日4次;萘普生250-5--mg,口服,日2次;吲哚美辛25mg,口服,日3次。分别应用这三种药物,如病情仍然没有改善可考虑全身应用类固醇。
2)全身应用类固醇 泼尼松60-100mg,口服,日1次,共1周,第2-3周逐渐减量到20mg,然后缓慢减量。加用非甾体类抗炎药配合类固醇减量。如类固醇效果不佳,可考虑免疫抑制剂治疗。全身应用类固醇之前,查看药物手册中“泼尼松”部分。
3)免疫抑制剂治疗 如环磷酰胺、甲氨蝶呤、环孢霉素A、硫唑嘌呤。如一种药物无效或不能耐受,应试用其他药物,可同时应用类固醇药物。免疫抑制治疗应由内科专家或类风湿病专家指导进行。局部滴用环孢霉素A的作用不确切。
(局部用药需谨慎)
2 Necrotizing scleritis:
—Systemic steroid and immunosuppressive therapies areused as above.
—Scleral patch grafting may be necessary if there issignificant risk of perforation.
2.坏死性巩膜炎
1)全身应用皮质类固醇药物和免疫抑制治疗,方法如前所述。
2)对于穿通性巩膜软化,应给与足量的润滑剂治疗。
3)如果有巩膜穿孔的危险,可给以巩膜植片移植修补术。
(原文2点,中文版3点)
3 Posteriorscleritis: Therapy is controversial and may include systemic aspirin, NSAIDs,steroids, or immunosuppressive therapy as described previously. Consult retinaspecialist.
3.后巩膜炎 对后巩膜炎的治疗尚有争议,可全身应用阿司匹林,非甾体抗炎药,类固醇药物或免疫抑制剂治疗,方法如前所述。
4 Infectious etiologies: Treatwith appropriate topical and systemic antimicrobials. Oral fluoroquinoloneshave good tissue penetration. If a foreign body [e.g., scleral buckle(associated with Proteus)] is present, surgical removal is indicated.
4.感染性病因 根据病情给与眼局部和全身以抗微生物药物治疗。口服氟喹诺酮的组织穿透性很好。如果有异物,如巩膜扣带(伴发变形菌属感染),应手术去除。
5 Glasses or eye shield should be worn at alltimes if there is significant thinning and perforation risk.
5.如巩膜有明显变薄或穿孔危险,应全天戴眼镜或眼罩。
Note
Topical steroids are not effective in scleritis.Although controversial, subconjunctival steroids are usually contraindicated,especially in necrotizing scleritis, and may lead to scleral thinning andperforation.
注:巩膜炎患者的眼局部应用类固醇无效。虽然有争议,但应禁用结膜下注射类固醇特别是在坏死性巩膜炎,可导致巩膜变薄和穿孔。
Follow-Up
Dependson the severity of the symptoms and the degree of scleral thinning. Decreasedpain is a sign of response to treatment, even if inflammation appearsunchanged.
随访:
随访的频率根据症状的严重程度和巩膜的变薄程度而定,尽管有时炎症反应未见明显变化,但疼痛减轻可提示治疗有效。